Insomnia is a sleep disorder that affects how easily a person falls asleep and how long they stay asleep. In the UAE, there is a high prevalence of insomnia. In fact, some studies indicate that up to 30 percent of people from the UAE experience insomnia at some point in their lives.1 Insomnia can be a symptom or a condition in itself. For example, there are illnesses, such as heart disease and sleep apnea, which can make it difficult to fall asleep. Mental conditions can also cause sleeplessness. For some people, what they experience is stress insomnia. This is when their stress levels are elevated enough to disrupt their usual sleep patterns .2

Why Stress Insomnia Matters
There are no set rules regarding the amount of sleep a person needs. It can depend on various factors such as activity levels and age. However, most adults need about seven to nine hours of sleep. It is also important to consider the quality of sleep, or how restful the sleep actually is.
It is important for people to understand that insomnia is a sleep disorder. In other words, it is more than a sleepless night. A person who has insomnia experiences a persistent pattern of difficulty falling or staying asleep. This happens even when they create opportunities for sleep. Over time, this lack of sleep makes it difficult to function normally.
Impact of Insomnia on ICU Nurses in Dubai
In 2023, a team of researchers conducted a study on the impact of insomnia on nurses in the UAE. Researchers asked 430 nurses from government hospital in the UAE and asked them about their work and the quality of their sleep. They found that work productivity and quality of life decrease with the presence of insomnia. Some of the reported effects are long-term health issues, cognitive impairment, and job dissatisfaction.3 Although the researchers noted that what they found was an association rather than causation, studies like these reinforce what most experts already believe. Those who experience insomnia can experience physical and mental challenges.
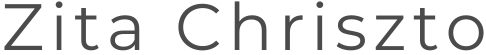
The study used convenient sampling methods to administer questionnaires to the ICU nurses. The Athens Insomnia Scale (AIS) was used to determine insomnia levels. This assessment records the participant’s sleep difficulty using eight questions. The individuals rate each question from zero to three. Zero means there is no problem, while three indicates a significant issue.
According to the data collected, 65.4% of the nurses had issues with sleeping induction, 79.1% reported issues with waking up in the middle of the night, and 75.7% reported issues with waking up too early. The results also showed 85.6% of the nurses were dissatisfied with their sleep duration, while 85% had overall low sleep quality. The AIS also rated the severity of the nurses’ insomnia. More than half were determined to have moderate to severe insomnia.
The Relationship Between Insomnia and Stress
Insomnia can either be short-term or chronic. Short-term insomnia is usually related to a distressing or stressful event. Some examples are work-related concerns or relationship issues. These stressors cause temporary sleep disruptions. Chronic, or long-term, insomnia, is related to persistent stressors. A person is diagnosed with chronic insomnia if they experience symptoms at least three times a week for at least three months. Chronic insomnia is usually due to persistent stressors.
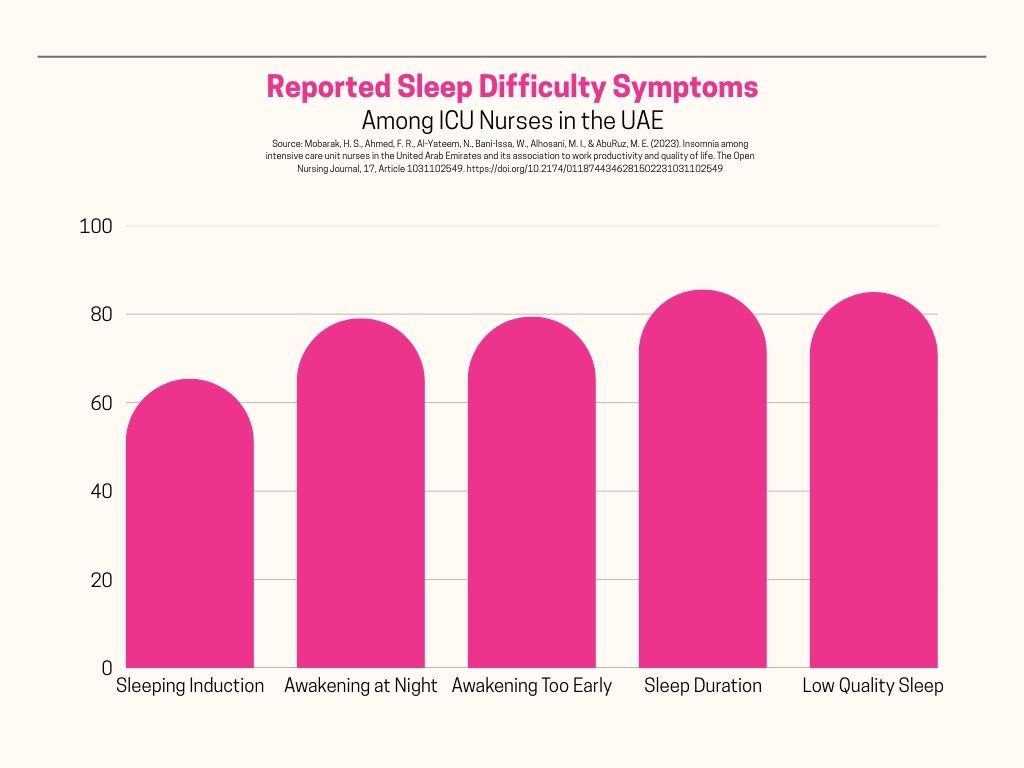
Sleep and stress have a reciprocal relationship. In other words, the presence of one leads to the other, and vice versa. When a person is stressed over a particular situation, emotions tend to run high. This means that feelings of anxiety, worry, or dread can be harder to control. This leads to overstimulation. Think about how you overthink during stressful situations. It does not stop even when you are tired. This overstimulation can make it difficult to sleep. Sleep deprivation then leads to increased cortisol levels, which can exacerbate stress levels even more. 4
Effects of Stress Insomnia on the Body
A day or two of sleeplessness probably will not make much of a difference in the body. However, long-term stress insomnia can have a significant impact on a person’s health.
Sleep Loss Affects Hormone Production
One way that insomnia affects the body is the production of hormones. For example, people who have short sleep durations tend to have higher body mass. One reason for this is that lack of sleep affects the hormones that control appetite. Lack of sleep is associated with the suppression of leptin, a hormone that reduces appetite. It also increases the production of ghrelin, a peptide that acts as an appetite stimulant.5
Insomnia can play a role in physical diseases. There are studies that associate sleep deficiency with insulin sensitivity, which can lead to type 2 diabetes. Insulin is a hormone that regulates blood sugar levels. When the body becomes resistant, the pancreas, which produces insulin, tries to manufacture more. If it cannot produce enough, then blood sugar levels rise.
Cardiovascular Issues Can Stem from Sleep Loss
There are some large-scale studies that link the lack of sleep with heart attacks and strokes.6 Although the exact reasons behind this link are still unknown, there are several possible explanations. One is the increase in blood pressure. Another possible reason is sympathetic hyperactivity. This describes a situation when the sympathetic nervous system, which is responsible for the fight or flight response, is overstimulated because of a lack of sleep. It can lead to elevated blood pressure and heart rate.7
Lack of Sleep and Mental Health Challenges
Chronic insomnia has a negative impact on mental health. It is linked with anxiety, depression, and alcohol abuse.8 There are many studies that create this association. However, it is difficult to determine the exact connection. The reason for this is the reciprocal nature of insomnia and stress. Stress is known to exacerbate symptoms in mental health conditions.
Interventions Addressing Stress Insomnia
Stress management is a lifeline for people going through stress insomnia. Cognitive behavioral therapy is often used. This type of therapy identifies how a person’s thoughts and beliefs influence their behavior and how they view the world.9 In short, the stressors remain, but you learn to react to them more positively.
There is also a more specific form of cognitive therapy that addresses insomnia. Called cognitive behavioral therapy for insomnia, its aim is to teach people to have a healthier outlook when it comes to sleep.10 It uses a combination of techniques such as relaxation strategies, sleep restriction, and coping strategies for stress. The Mayo Clinic outlines some of the strategies usually employed. Some of the examples given are stimulus control therapy and relaxation methods.
Medication is also used to address insomnia. These prescription sleeping pills work in different ways. Some help you fall asleep faster. Others help you stay asleep. Others address both issues. The benefits are different, and so are the risks. This is why it is important to take medication with the guidance of a health professional.
Before a doctor prescribes medication, they first determine the patient’s sleeping patterns. Underlying conditions are also ruled out. Prescription sleeping pills have side effects such as grogginess and unsteadiness. It is also possible for it to be habit-forming. The doctor will typically prescribe medication for a short time, then assess how the patient reacts to it.
Conclusion: A Common Sleep Disorder with Serious Effects
Insomnia is fairly common. Most studies place the number at about 10 to 30 percent of the population worldwide.11 However, just because it is prevalent does not mean it should be ignored. It can have serious effects that range from low energy levels to increased risks of disease and mental health conditions.
Stressors can trigger insomnia. Sometimes this stressful event can last for longer periods and affect a person’s sleep patterns much longer as well. If quality of life is affected, it is important to find ways to address the sleep loss. A person can try lifestyle changes such as maintaining a sleep schedule or making their sleeping areas more restful. However, it is also helpful to seek out the help of a medical professional to rule out medical causes of insomnia. Some other interventions to explore are therapy, medication, or both.
Sources Cited:
- Asma Ali Zain. (2018, June 23). 30 % of UAE residents experience insomnia for certain period. Khaleej Times. https://www.khaleejtimes.com/uae/30-of-uae-residents-experience-insomnia-for-certain-period ↩︎
- Shaheen, S.H., Abdullah, E.A., Razik, M.M.A. et al. Prevalence of insomnia in a sample of Internet addicts in different age groups in Abu Dhabi, UAE. Middle East Curr Psychiatry Mobarak, H. S., Ahmed, F. R., Al-Yateem, N., Bani-Issa, W., Alhosani, M. I., & AbuRuz, M. E. (2023). Insomnia among intensive care unit nurses in the United Arab Emirates and its association to work productivity and quality of life. The Open Nursing Journal, 17, Article 1031102549. https://doi.org/10.2174/0118744346281502231031102549, 27 (2023). https://doi.org/10.1186/s43045-023-00301-9 ↩︎
- Mobarak, H. S., Ahmed, F. R., Al-Yateem, N., Bani-Issa, W., Alhosani, M. I., & AbuRuz, M. E. (2023). Insomnia among intensive care unit nurses in the United Arab Emirates and its association to work productivity and quality of life. The Open Nursing Journal, 17, Article 1031102549. https://doi.org/10.2174/0118744346281502231031102549 ↩︎
- Hanson JA, Huecker MR. Sleep Deprivation. [Updated 2023 Jun 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK547676/ ↩︎
- Institute of Medicine (US) Committee on Sleep Medicine and Research; Colten HR, Altevogt BM, editors. Sleep Disorders and Sleep Deprivation: An Unmet Public Health Problem. Washington (DC): National Academies Press (US); 2006. 3, Extent and Health Consequences of Chronic Sleep Loss and Sleep Disorders. Available from: https://www.ncbi.nlm.nih.gov/books/NBK19961 ↩︎
- Eaker ED, Pinsky J, Castelli WP. Myocardial infarction and coronary death among women: Psychosocial predictors from a 20-year follow-up of women in the Framingham Study. American Journal of Epidemiology. 1992;135(8):854–864. ↩︎
- Liu Y, Tanaka H. Fukuoka Heart Study Group. Overtime work, insufficient sleep, and risk of non-fatal acute myocardial infarction in Japanese men. Occupational and Environmental Medicine. 2002;59(7):447–451. ↩︎
- Strine TW, Chapman DP. Associations of frequent sleep insufficiency with health-related quality of life and health behaviors. Sleep Medicine. 2005;6(1):23–27. ↩︎
- Lopez, C., Antoni, M., Penedo, F., Weiss, D., Cruess, S., Segotas, M. C., Helder, L., Siegel, S., Klimas, N., & Fletcher, M. A. (2011). A pilot study of cognitive behavioral stress management effects on stress, quality of life, and symptoms in persons with chronic fatigue syndrome. Journal of psychosomatic research, 70(4), 328–334.
https://pubmed.ncbi.nlm.nih.gov/21414452/ ↩︎ - Schwab, R. J. (2022, May). Insomnia and excessive daytime sleepiness (EDS). Merck Manual Consumer Version., Retrieved February 1, 2023, from
https://www.merckmanuals.com/home/brain,-spinal-cord,-and-nerve-disorders/sleep-disorders/insomnia-and-excessive-daytime-sleepiness-eds ↩︎ - Bhaskar S, Hemavathy D, Prasad S. Prevalence of chronic insomnia in adult patients and its correlation with medical comorbidities. J Family Med Prim Care. 2016 Oct-Dec;5(4):780-784. doi: 10.4103/2249-4863.201153. PMID: 28348990; PMCID: PMC5353813. ↩︎